Hospital Initiatives Help Fight Healthcare’s Biggest Challenge – Chronic Disease
By Betsy Ryan, Esq., President and CEO of the New Jersey Hospital Association On Dec 1, 2015Take a look at some of the biggest challenges confronting our healthcare system, and you’ll find chronic healthcare conditions play a major contributing role. Rising healthcare costs? Check. Hospital readmissions? Check. Lost productivity and reduced quality of life? Check.
Americans are living longer, and the Baby Boomer generation is creating a swell of aging healthcare consumers. The resulting rise in chronic health conditions – things like arthritis, heart disease, diabetes and more – places a tremendous burden on our hospitals and other healthcare providers.
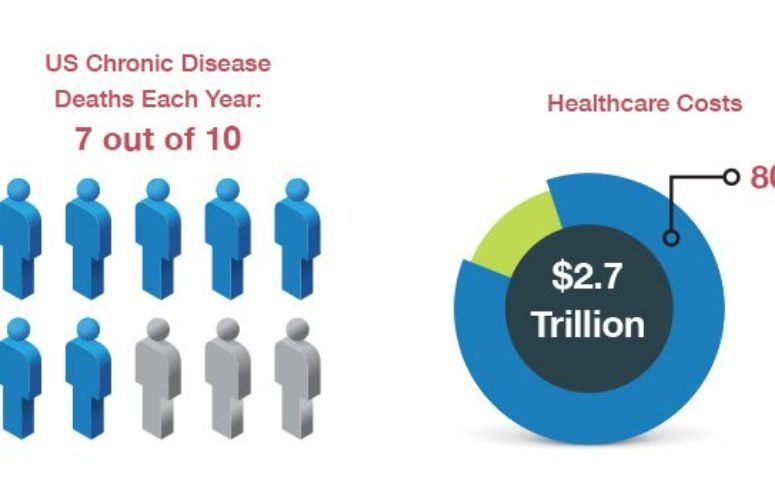
Chronic diseases are responsible for 7 out of 10 deaths in the United States each year, according to the Centers for Disease Control and Prevention, and they also account for more than 80 percent of the $2.7 trillion in US healthcare costs each year. For the 133 million Americans living with chronic conditions, limited functional status, productivity and quality of life is a daily reality.
This isn’t just a healthcare concern; it’s a societal issue.
At the New Jersey Hospital Association (NJHA), we’ve launched a number of initiatives over the past decade to confront chronic conditions. Two major projects under the NJHA Institute for Quality and Patient Safety include “Expecting Success,” which developed quality improvement strategies, models and resources to improve cardiac care for African-American and Hispanic/Latino patients diagnosed with heart failure, and “Dulce New Jersey,” which worked to improve diabetes care and outcomes through two major strategies: nurse-managed clinical care and community-based diabetes education and health promotion. (Incidentally, both initiatives also targeted another ongoing challenge in public health – health disparities among different ethnic and racial groups.)
While our initiatives focused largely on what healthcare providers can do to improve chronic disease care, it was all too apparent that what happens elsewhere – in the home or in the community – has a significant influence on chronic disease. As we talked to diabetics about the importance of maintaining a healthy weight, we heard from many that didn’t have a scale in their homes. And as we counseled heart disease patients to avoid fats and eat a healthier diet, they told us there was no grocery store in their community to buy fresh foods. (It’s a growing problem in many areas, and there’s even a name for it – “food deserts.”)
We’re facing very similar issues as hospitals work to reduce the number of people who are readmitted to the hospital within 30 days of a prior inpatient stay. The Affordable Care Act carries financial penalties for hospitals when readmission rates exceed the federal government’s targets. However, we know that community factors play a significant role in ensuring that a patient’s recovery remains on track following a hospital stay – things like access to primary care services, public transportation to medical appointments and financial considerations such as prescription costs and insurance co-pays.
As the population ages, we’re also seeing an increase in mental health conditions, including depression, substance abuse and dementia. Those older adults may be isolated, without family or support, and on fixed incomes. The need is great for additional resources from nurses, social workers, rehab specialists and behavioral health counselors.
It will take a holistic approach to reduce the burden of chronic disease, with an array of partners – healthcare providers certainly, but also state and local government, schools, social services and individuals – working together to achieve the goal of living well with chronic illness.
Related Articles: