Pushing Medical Boundaries in Fight Against COVID-19
Hospital and med-tech firms address new maladies and adopt different strategies to tackle familiar illnesses.
By João-Pierre S. Ruth, Contributing Writer On Jun 11, 2020The state’s ongoing efforts to advance medical technology and healthcare delivery hold new relevance in the treatment of diseases such as COVID-19. Healthcare systems such as Hackensack Meridian Health and Valley Health System found themselves on the frontlines of treating patients affected by the pandemic. Meanwhile, St. Peter’s Healthcare System, with its designated Regional Perinatal Center, has taken expert precautions ensuring the proper delivery of medical services to expecting mothers who have contracted COVID-19, both during prenatal visits and births.
On the diagnostic side of the healthcare spectrum, Ortho Clinical Diagnostics got to work developing a test for antibodies that fight the disease.
The crisis set off by the pandemic highlights the resources for medical innovation gathered in New Jersey that could lead to relief beyond the state’s borders.
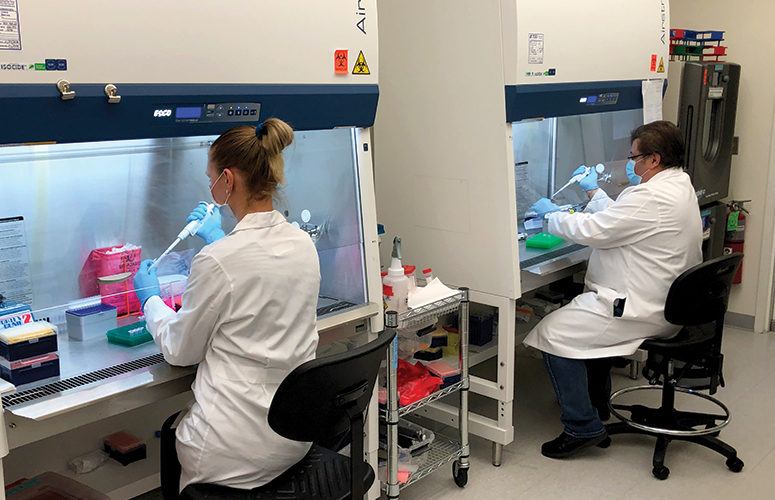
Research efforts at Hackensack Meridian Health’s Center for Discovery and Innovation (CDI) leverage high-end, molecular science to improve outcomes for patients with cancer, infectious diseases, and other acute and chronic diseases, says David Perlin, chief scientific officer. The increasing availability of novel medical resources, he says, can lead to expanded possibilities in treatment. He explains, “We can make these tools work in real-time for patients.”
For example, Perlin says CDI’s efforts in oncology include looking at blood cancers, solid tumors, and new ways to diagnose and treat those cancers through cell-based and conventional therapies. That can mean advancing recent innovations in science as quickly as possible to trial phases. Clinical needs drive the science, he says, which can differ from the academic realm where scientific discovery is often about innovation in search of diseases.
CDI works in partnership with the John Theurer Cancer Center, one of the largest centers of its kind in the region, pharmaceutical and biotech companies, academic researchers, and clinicians. “We want to work in this mixed ecosystem whether the innovation is coming from a company or our laboratories so that we can move it into the clinic,” Perlin says.
Ongoing programs at CDI include exploring treatments for bone cancers and hematologic malignancies using new types of cell therapy, he says. Though CDI has only been organized for about a year, he says it has more than 90 grants and contracts in its portfolio, including partnership grants with companies to solve problems in oncology and infectious disease.
Addressing infectious diseases includes searching for ways to arrest healthcare-associated infections, which can occur in patients who are immunocompromised due to transplantation, cancer and other causes. “The first thing is to understand what the flow of infectious agents within our system is,” Perlin says. “Who’s becoming infected? Where are the high-risk points? Then put in strategies to reduce those infections.”
The emergence of the COVID-19 pandemic meant CDI’s expertise needed to be put to work at a rapid pace. “We approached this early on assuming that the biggest challenge was going to be testing,” Perlin says. “I’ve been involved in epidemics for anthrax, H1N1 and multidrug resistant infections.” CDI put in place a diagnostic platform using molecular technology, he says, that was ready by the beginning of February. However, it took another three weeks to validate the panels due to delays in getting validating materials, Perlin says.
Molecular testing for COVID-19 allows for triage of patients, he says, and directing resources where most needed. Drug discovery programs are underway, Perlin says, with major pharmaceutical companies to screen for existing drugs that may be active against the virus. The effort will also explore and identify new molecules that could be active versus COVID-19. “That’s a longer-term program,” he says. The ongoing mission is to identify patients with antibodies, qualify them, and get them ready so clinical teams can use them in therapy.
Keeping abreast of the influx of COVID-19 patients and treatment has been taxing for many hospitals. It has also led to some creative adaptations to cope with the situation. Valley Health, for example, says a shortage of disposable gowns forced its staff to launder 1,000 to 2,000 reusable gowns on a nightly basis. The hospital’s departments of facilities and engineering – within one week – converted one of its units into negative pressure rooms, which prevents cross-contamination in a facility.
“Our staff has gone above and beyond to address the challenges presented by this pandemic,” says Robert Brenner, president of clinical integration and physician enterprise at Valley Health System. “People have stepped up to take on new roles as needs change, and have shown an incredible strength in dealing with a very difficult situation.”
Meanwhile, St. Peter’s Healthcare System’s designated Regional Perinatal Center is providing exceptional high-risk maternity care for women and their babies during the pandemic. On the outpatient side, prenatal visits are recommended only after women have been screened and deemed to be at low risk for COVID-19 infection. A phone screening the day before an appointment asks specific questions regarding signs and symptoms associated with COVID-19. When possible, telemedicine and other technologies are used to reduce the risk of exposure posed by face-to-face meetings.
For inpatient maternity care, all expectant mothers are screened for COVID-19 symptoms before admission. If the patient screens negative, standard precautions to reduce infection risk are put in place, such as handwashing, respiratory etiquette and masking by both patients and providers.
If patients screen positive, they are isolated in specific areas where they can be monitored and treated. Special care teams have been created to deal with maternity patients who present with the virus. The teams consist of infectious disease and pulmonary critical care specialists that evaluate and care for patients with the infection. A team, including a neonatologist and a pediatric infectious disease physician, cares for newborns whose mothers have a confirmed diagnosis.
An infant born to a mother with a known or suspected infection is separated from the mother until it is deemed safe for the infant.
“We are very sensitive to the fact that this is a difficult transition for the mother, but it is the safest thing to do,” says Leslie D. Hirsch, president and CEO of Saint Peter’s Healthcare System.
The testing aspect of getting the pandemic under control is a focus for Ortho Clinical Diagnostics. In April, the company announced the launch to market of its antibody test called the VITROS Immunodiagnostic Products Anti-SARS-CoV-2 Total Reagent Pack, which detects antibodies in an immune response to the COVID-19 virus. Chockalingam Palaniappan, chief innovation officer, says the tests are designed to run on Ortho’s analyzers, which are already in place at more than 1,000 labs and hospitals across country.
Palaniappan says not everyone exposed to or infected with the virus will experience the full severity of the disease. Ortho’s test for immunity, which would reveal the presence of the virus even without obvious symptoms, is done through a blood draw. Other companies have been testing for presence of the virus through nasal swabs. Ortho has experience with antibody, serological tests to monitor human immune response, Palaniappan says. The company has developed such tests for HIV, hepatitis and others viruses.
The Food and Drug Administration authorized Ortho to commercialize its serological test for COVID-19 immunity and the intent is to use the testing kits with diagnostic machines already in the field. Those machines can process 150 samples in one hour, Palaniappan says, with fully automated reporting of results. “A single machine could perform 3,500 tests per day if it only tests for COVID-19,” he says. If 1,500 machines were to run the tests, he says it may be possible to perform 4 million to 5 million tests per day in the US. Ortho planned to have millions of test kits available the by end of May-early June, Palaniappan says. “Testing is one of the key tools used in making decisions around getting people back to work.”
To access more business news, visit NJB News Now.
Related Articles:





