Depression’s Dramatic Rise
Healthcare experts discuss why there is such a dramatic increase in cases and what is being done to fight the illness.
By Anthony Birritteri, Editor-in-Chief On Nov 11, 2019Healthcare professionals have seen a steep rise in depression over the last few years. Among the causes for the increase, based on the personal beliefs of a number of New Jersey experts, are the increased use of smart phones and social media, which is limiting face-to-face human interactions, and in turn, increasing feelings of isolation. Additionally, social media postings of presumed “idyllic” lifestyles can make online followers feel like their own lives, in comparison, are somewhat lacking in elements such as success, wealth, friendship and adventure, in turn generating feelings of depression.
Other factors causing depression rates to increase may include the 24/7 news cycle that, for example, feeds the fire of vitriolic political banter and, tragically, mass shootings and terrorist attacks. Add to the mix workplace scenarios such as doing more with less staff and/or working around the clock thanks to technology that keeps us connected 24/7, and one sees stress and anxiety levels increasing, which in the long-term gives rise to episodes of depression.
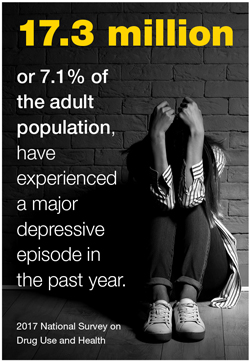
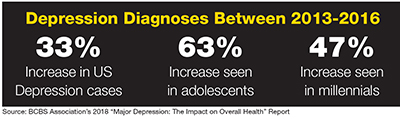
Debra Wentz, president and CEO of the New Jersey Association of Mental Health & Addiction Agencies (NJAMHAA), reports that, based on a Blue Cross Blue Shield Association report titled “Major Depression: The Impact on Overall Health,” cases of depression in the US increased by 33% between 2013 and 2016. And according to data from a 2017 National Survey on Drug Use and Health, approximately 17.3 million US adults, or 7.1% of the adult population, have experienced a major depressive episode in the past year.
In a strongly related statistic, suicide is also on the rise in the US, increasing by 30% between 2000 and 2016. According to Christopher Saslo, DO (Doctor of Osteopathy), psychiatrist and medical director of Capital Health System’s Psychiatric Screening Center in Trenton, “Every year, 13.4 people out of 100,000 commit suicide in the US.” If one would consider the next statistic a bright spot, it is that New Jersey’s rate is 7.17 people per 100,000. Saslo credits the lower rate to the state’s vast array of quality behavioral health services.
The Social Media Factor
“One of the problems with social media,” Wentz says, “is that people will only post carefully curated photos to their feeds, showing that they are leading a perfect life. When someone with poor self-esteem sees others living carefree, drama-free lives, it causes them to feel poorly about themselves. … That, in turn, is related to depressive symptoms.”
According to Don Parker, president of Carrier Clinic and head of Hackensack Meridian Health’s Behavioral Health Care Transformation Services, “Everyone is talking about the impact and increased usage of smart phones. My hypothesis is that the subtraction of body language from the exchange may have some type of biochemical effect on the body. In psychology class, one is taught that 65% of all communications is nonverbal. If you do 50% or more of your communications on the cell phone today, your body language intake is reduced by 50% … so you are not seeing the physical signs, for example, of empathy, sympathy and understanding. … In a lifetime, what does the accumulation of those missing elements do to you?”
NJAMHAA’s Wentz says the 24/7 news cycle is another factor contributing to depression. “In 2017, a survey by the American Psychological Association reported that American politics and acts of terrorism and violence were activating stress triggers,” she says, adding that Maryland-based therapist Dr. Steven Stosny coined the phrase “headline stress disorder” to describe what was happening.
Even more dangerous is the fact that violent headlines are influencing people with other types of behavioral health issues to conduct acts of violence because they see the headlines and news reports as “glorifying” the killers. “It draws people with certain kinds of illnesses into that. It can promote that behavior in the wrong people,” Saslo comments.
Workplace Issues
Workplace stress can also lead to depression. Earlier this year, the World Health Organization even declared unmanaged stress on the job an occupational health issue. “Stress leads to burnout, which leads to exhaustion, lethargy, reduced efficiency, negative and cynical thinking, which has a significant impact on an individual’s mental and overall health,” Wentz says.
“It is important for employers and employees to set limits and boundaries regarding work and not, for example, bring stress home,” she continues, adding that as much as 70% of full-time employees will experience a major depression and that the illness is a leading cause of absenteeism. Overall, she says that mental illness is the leading cause of disability in the US, costing the economy approximately $200 billion a year, based on National Alliance on Mental Illness statistics.
Because a stigma still exists for those suffering from a mental illness, employees may not disclose that they suffer from depression, for example, for fear it would harm their careers, Wentz says. A Kaiser Permanente (KP) report reveals that workers with mental health conditions delay seeking treatment for up to 8 to 10 years due to the stigma fear. Because of that, “it’s critical to have a stigma-free work environment because employees would be more aware of the resources available to them and seek treatment sooner rather than later, leading to increased productivity and positive outcomes,” Wentz says.
Plans of Action
New Jersey’s healthcare systems are making new inroads in how to treat depression, whether it is through strategic mergers, new facilities or better community outreach.
Among the many examples of enhanced services is Hackensack Meridian Health’s (HMH) merger with Carrier Clinic this past January.
Explaining the reason for the union, HMH President Bob Garret tells New Jersey Business, “We are trying to incorporate behavioral health into our medical protocols because so many patients who have other medical issues have behavioral health problems.”
Carrier Clinic, based in Belle Mead, has a 100-year history in the state. With nearly 1,100 team members, Parker explains the merger now delivers 3,500 people within the HMH system working in behavioral health. He says, “Carrier had been on a journey to become a tertiary and premier behavioral healthcare provider. So, we needed to connect ourselves to an educational program, to a research institution and a health system that would offer the reach to serve multiple audiences.”
Among the first developments of the merger was the recent opening of an HMH urgent care center with behavioral health services in Neptune. According to HMH, the center offers patients access to a behavioral health team that: treats them in an appropriate setting; provides more timely care for people who need to see a specialist; reduces the burden on already stressed emergency room departments; and gives patients a safe and confidential place to seek care (addressing the stigma issue).
The merger between HMH and Carrier is also expected to result in the opening of new addiction treatment centers, and a $25-million upgrade for Carrier’s Belle Mead campus.
Discussing the long list of behavioral health services at Capital Health, Saslo mentions the system’s newest offering: an outpatient psychiatry practice in Hamilton. Staffed with two full-time psychiatrists and one part-time, he says the facility is looking to increase its staff size because of the positive community response.
Meanwhile, the majority of Capital Health’s psychiatric services are offered at Regional Medical Center in Trenton, which has an inpatient psychiatric unit consisting of 26 beds. Additionally, behavioral health consultations occur at Capital Health Medical Center in Hopewell.
One of the services Saslo is most proud of is the “Psychiatric Screening Center at Mercer County. This is where we do lot of our community outreach. It is basically a separated unit from the ER, but it’s connected for patients undergoing psychiatric emergencies or crises. We try to stabilize the patient and discharge them within an appropriate level of service. If necessary, we help get them into a hospital where they can get further treatment.”
Government Intervention
Most recently, federal and state governments have also been playing major roles in making sure people get access to adequate behavioral healthcare services. NJAMHAA’s Wentz says she is excited about New Jersey being one of eight states involved in a federal two-year pilot program for certified community behavioral health centers. “The centers have received enhanced Medicaid reimbursement rates based on their anticipated cost of care, and were able to contract with partner organizations to provide an array of mental health services,” she says.
Funding for the program sunset this past June, but it has received extensions through continuing resolution appropriations up until November 21. Wentz says NJAMHAA has been actively advocating for its continuation.
She was also glad to see Governor Murphy sign into law this past April a mental health parity bill (A2031/S1339) that requires health insurers to provide coverage for mental health conditions and substance use disorders under the same terms and conditions as provided for any other sickness and to meet the requirements of the federal Mental Health Parity and Addiction Equity Act of 2008.
Conclusion
Obviously, smart phones, social media, and a stressful workplaces should not solely be blamed for the increase in depression. As Saslo says, depression seems to be the result of “a combination of biological, psychological and social factors.”
He adds, “If we know we are at risk, we can try to take good medical care of ourselves (eat, exercise, undergo preventive healthcare checks) and try to avoid substance abuse.”
Though there is a shortage of psychiatrists and other behavioral healthcare professionals in the US and New Jersey, the outlook for quality behavioral health treatment in the state is positive, as Saslo comments, “There are a ton of different organizations and clinics that offer psychiatric care. … All we want is for people to have access to services when they really need them.”
To access more business news, visit NJB News Now.
Related Articles: