The Conflict Between Cost and Coverage
In Action on Healthcare
By Mary Beaumont, NJBIA Vice President of Health & Legal Affairs On Aug 30, 2017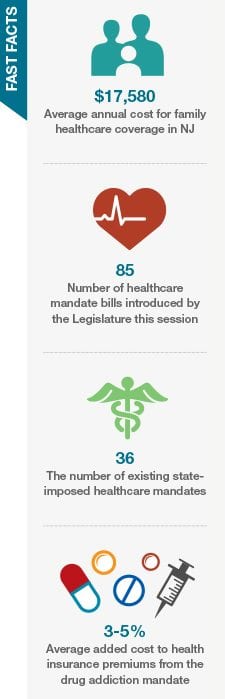
While mandates are not the only cause for rising health insurance costs, they do contribute to the problem. That’s why NJBIA strives to find a balance between the cost and the benefit of individual proposals.
Mandated Health Benefits Advisory Commission. NJBIA advocated for an objective review of healthcare mandates’ costs and the likely benefits they will produce. In 2003, legislation was signed creating the Mandated Health Benefits Advisory Commission (MHBC) to review the social, financial and medical impact of any mandated health benefit legislation before it is voted on. The commission includes representatives from the business community, including NJBIA, and the medical community.
The commission’s role is critical. NJBIA has consistently opposed mandate legislation that has not been reviewed by the commission. In 2017, NJBIA is following 20 bills mandating specific health coverages, but only one of them has received a full analysis.
Abuse-deterrent Drugs. The one bill that was analyzed shows the importance of having independent, objective information for such legislation. S-1313 would mandate coverage for opiates with abuse-deterrent properties. With opioid addiction at the forefront of New Jersey’s health issues, the bill passed both houses with substantial majorities, even though it had not been referred to the commission. Fortunately, Gov. Chris Christie vetoed the bill.
The bill was then referred to the MHBC, which concluded that such abuse deterrents were not by themselves a solution to the problem because addicts would simply turn to cheaper and easier alternatives. The MHBC concluded it would have resulted in higher health insurance costs if this bill had become law.
Substance Abuse Treatment. One healthcare mandate that was enacted this year extends the length of drug rehabilitation programs that insurance must cover. New Jersey became the only state in which people with insurance are guaranteed coverage and cannot be retroactively charged for six months of needed treatment. Under the law, people diagnosed with a substance abuse disorder will have covered treatment for 180 days.
Other Mandates. While drug addiction mandates have a broad impact, most insurance mandates are more narrowly focused. In June, legislators voted to mandate all contraceptive prescriptions be written for a 12-month period. Governor Christie conditionally vetoed the measure, requesting the time period be cut to six months, to prevent prescription drug waste and contain costs.
Related Articles: