Hospitals Deliver Quality Care to Patients
Despite challenges facing the industry, the state’s healthcare networks continue to improve quality care and safety outcomes for patients within their facilities.
By Jennifer Lesser, Contributing Writer On Oct 23, 2017New Jersey’s healthcare industry has dealt with a long list of challenges in recent months, from ongoing uncertainty regarding healthcare reform in Washington, DC, to legal battles over property taxes within its own communities. But the state’s hospitals continue to meet the ever-changing demands of the healthcare industry while improving the level of quality care and safety delivered to patients.
According to Linda Schwimmer, president and CEO of the New Jersey Healthcare Quality Institute, the state’s healthcare networks are working hard to make improvements in several areas that directly affect quality care, including lowering the caesarean section rate, earlier identification and treatment of sepsis infections, and reducing hospital readmissions. She notes that local hospitals are addressing the fact that New Jersey has some of the highest rates of caesarean sections in the country, and are turning their attention to enhancing strategies for early identification and treatment protocols to treat sepsis within three hours, which has a dramatic impact on saving lives.
“Over the past several years, hospitals have also been very focused on reducing their readmission rates by constantly striving to improve the transition for patients between the hospital to their other healthcare providers, from physicians to skilled nursing facilities,” she adds.
Hospitals like CentraState Healthcare System are participating in collaborative groups designed to identify best practices within the industry, such as lowering rates of sepsis in order to improve the level of care they’re delivering to patients within their facilities. “It’s beneficial for us and all of the hospitals throughout New Jersey. Over the last 10 years, there has been a dramatic improvement in quality and safety measures for the state, and we believe these collaborative groups are a significant factor in identifying issues and improving our processes to enhance our quality of care,” John T. Gribbin, CEO of CentraState Healthcare System, says.
In the meantime, the state’s hospitals are adhering to an ever-increasing demand to be more transparent. “It’s been a big change in New Jersey over the last few years … hospitals are more willing to become fully transparent about their quality,” Schwimmer says, noting that nearly all of the state’s hospitals are voluntarily sharing data with Leapfrog and organizations that report on hospital safety and help consumers make educated decisions about their healthcare.
“We are committed to full transparency to help patients make the most informed decisions, and for our teams to monitor outcomes,” John K. Lloyd, co-CEO of Hackensack Meridian Health, asserts. For example, the vast majority of the system’s hospitals have rates of catheter-associated urinary tract infections that are lower than state averages, and more than half of Hackensack Meridian’s hospitals have central line-associated bloodstream infection rates lower than the national average. “These bloodstream infections result in thousands of deaths in the United States each year, and add billions to our nation’s healthcare costs – and they’re entirely preventable,” Lloyd adds. “That’s why we’re working constantly to ensure patients receive the highest quality care in the safest environment.”
Like many of the state’s hospitals, Hackensack Meridian Health is also aggressively monitoring quality measures, such as rates of infection, readmission and patient satisfaction, and sharing those scores both internally with their team as well as online for the benefit of patients. This scorecard is reviewed at monthly operations meetings and with multi-disciplinary teams to determine what’s working and what needs improvement, Lloyd notes.
“Our network is always striving for new ways to be nimble, and to adapt to the challenges we face in finding better treatment, more convenient and cost-effective care, and more ways than ever to keep people healthy,” Robert C. Garrett, co-CEO of Hackensack Meridian Health, adds. “That includes constantly upgrading technology, treatment protocols, and the patient experience to provide the highest standard of care.”
Healthcare networks like Kennedy Health are also continuing to make safety and quality their No. 1 priority by enforcing a change in culture throughout their organizations, such as senior leadership enrolling in courses dedicated to topics like the importance of collaboration or how to put patients first. “You need an overall commitment to making quality your No. 1 priority … it’s something we don’t take lightly,” Dr. David Condoluci, chief patient and safety officer for Kennedy Healt, asserts. “We’ve embarked on the process of measuring everything and reporting our data to organizations like Leapfrog to see where we compare in everything from mortality and infection to readmission and patient satisfaction rates. We look at all of these things and continually set new goals to improve our quality of care.”
According to Dr. John Matsinger, executive vice president and chief clinical officer of Virtua, the hospital is also participating in an array of quality collaborative groups to help hone in on various safety-improvement measures. “On both the national and state level, we’re taking part in health engagement networks that are coming together to tackle issues like preventing sepsis or improving end-of-life care,” he explains.
One such example is the New Jersey Hospital Association’s (NJHA) recent High Reliability Organization Collaborative. “It selected 10 facilities across the state to pursue a zero-harm culture for patients,” Matsinger explains. According to the NJHA, high-reliability organizations are complex, high-risk organizations that always deliver the right outcome, despite human error and potentially unsafe systems and processes.
“Being a high reliability organization means that we always put safety first,” John DiAngelo, CEO of Inspira Health Network, explains. “Our three goals have always been to do no harm, deliver the best quality of care we can, and provide a healthcare experience that exceeds patients’ expectations. Now, we’re training thousands of employees to meet new standards that will help us to deliver an even higher quality of care than before.”
One such example is that the hospital has safety briefings every day, which give all physicians and anyone working directly with patients the opportunity to come together to discuss concerns that may require assistance in addressing immediately. “Our view is that whether it’s a staff member working in food service or housekeeping, or a doctor or nurse, anyone who is interacting with our patients in any way needs to have access to all of the resources that we have at their disposal,” DiAngelo adds.
CentraState is also among the 10 hospitals that received a grant to adopt high-reliability ideals. “It’s a concept that entered the healthcare field from other industries that are also considered dangerous or high-risk, and there’s a whole body of evidence that has developed with regards to the benefit of becoming a high-reliability organization,” Gribbin explains. “It’s a very encouraging phenomenon, and we’re embarking on a multi-year collaborative that will help us examine why mistakes happen in a healthcare organization and what we can do to continue to minimize that risk for our patients.”
Another major focus of hospitals as they strive to improve their level of quality care is addressing ongoing issues within the industry, such as the overuse of both antibiotics and opiates. “Our hospitals are taking on the responsibility of ensuring that we aren’t producing superbugs by prescribing antibiotics too aggressively, and due to a heightened awareness of the dangers associated with opiates, they’re looking at alternatives,” Schwimmer explains.
Perhaps the biggest buzzword in today’s healthcare industry is the concept of population health, which is playing an important role in helping hospitals hone in on what needs to be done in order to improve the quality of care they can offer within their communities. Today’s hospitals realize that they are more than just a facility that cares for people when they’re sick, which is a big part of the reason that the state’s healthcare systems now span a network of hospitals, private physician practices, urgent care centers, and other facilities designed to provide greater access to patients.
“We’ve had to restructure the way we do everything, and our ultimate goal is population health, which is all about trying to keep your community well,” DiAngelo says. These efforts run the gamut, from community health fairs to Inspira’s new wearable technology that can transmit a patient’s health-related data, such as their weight, directly to their physician to alert them to potential health issues before it happens. “Our goal continues to be to make life as simple as possible for the community we serve, and above all else, try to keep people well … not wait until they’re sick and have to come into one of our hospitals,” DiAngelo adds.
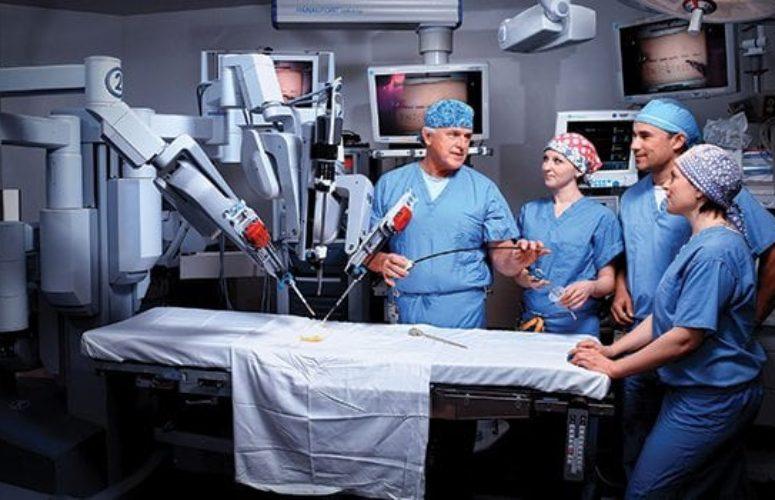
Of course, rapid advances in technology also play a crucial role in helping hospitals deliver quality care and improve safety outcomes for their patients. From the latest advances in electronic medical records to streamline a patient’s continuum of care to cutting-edge robotic surgeries to enhance precision and positive outcomes in the operating room, the state’s hospitals continue to adopt state-of-the-art technologies in order to deliver the highest level of care for patients.
“Technology – or, specifically, information technology – plays a major role in all of this,” Gribbin asserts. He notes that electronic medical records have made a significant impact in how physicians make the best possible decisions for their patients, while newer processes like barcoding for medications have also significantly decreased errors within the hospital. “Then you have robotic surgery, which is almost becoming the norm … it has enabled us to perform more complex surgeries with greater precision,” he adds.
The prevalence of electronic medical records has also paved the way for innovations like telemedicine to provide clinical care to patients from a distance. “Telemedicine has given patients access to their healthcare providers 24 hours a day, seven days a week, like the mother who’s at home with a small child and needs access to a physician right away. These are the kinds of technologies we’re pursuing to improve our patient experience,” Joe Wilkins, senior vice president and chief transformation officer for Atlantic Health System, explains. “We believe that electronic medical records have impacted the healthcare technology of the future in a major way, as we strive to have one record for each patient to maximize connectivity throughout a network of many different providers … and all while giving patients access to their records so they can better care for themselves.”
At Valley Hospital, advancements in technology are helping physicians treat patients more safely and effectively, particularly cancer patients at Valley-Mount Sinai Comprehensive Cancer Care, thanks to innovations like Deep Inspiration Breath Hold (DIBH) and a new therapy, Intraoperative Radiation Therapy (IORT), which is being offered as of this fall. The DIBH technique uses a woman’s breathing patterns to limit radiation exposure to the heart.
“Approximately 80 percent of patients with breast cancer will require radiation, but over the course of their lifetime, it increases the risk for heart disease. We’re using a technology that will significantly lower that risk,” explains Dr. Chad DeYoung, co-director of radiation oncology at Valley-Mount Sinai Comprehensive Cancer Care.
Meanwhile, the brand-new IORT for breast cancer patients delivers an entire course of radiation therapy to the patient while they’re in the operating room undergoing a lumpectomy – thereby eliminating the need for what is often several weeks of post-surgery radiation.
“Throughout our institution, we’re focused on streamlining and coordinating care and making sure patients receive the highest quality of care … and these technologies represent a major step forward towards those goals,” Dr. Michael Wesson, co-director of radiation oncology at Valley-Mount Sinai Comprehensive Cancer Care, adds.
Other facilities are expanding their roles as both educators and navigators in addition to providing medical treatment in their efforts to deliver better care to cancer patients. “To me, quality care means not only giving the best possible treatments and the access to cutting-edge clinical trials, but combining that with compassion and understanding of what the patient is going through as best you can. That means providing efficient care by a multi-disciplinary team that communicates with each other and offers patients a solid treatment plan,” Dr. Steven K. Libutti, director of the Rutgers Cancer Institute of New Jersey and senior vice president of oncology services for RWJBarnabas Health, says. “All medical treatments have inherent risk, but we’re doing our part to identify potential issues and de-risk these treatments as best we can.”
Looking ahead, the state’s healthcare systems know there will continue to be challenges as patients continue to demand the highest quality care and the most affordable, convenient treatment options, but they’re doing their part to continue to improve care and minimize negative outcomes.
“We know now that good health doesn’t just happen inside the walls of a hospital, and we won’t have any impact on the rising cost of healthcare or our nation’s chronic health issues if we stay inside our facilities. It’s our responsibility to go out and partner with our communities to affect factors that guide people’s health, such as proper diet and exercise,” Wilkins concludes.
Emergency Dept. Sees $18.7-M Renovation
Trinitas ER increases beds from 27 to 45.
Delivering emergency care more quickly, and with higher quality, is the aim of Trinitas Regional Medical Center, which recently completed an $18.7-million renovation and expansion of its Emergency Department. The 24,000-square-foot project raises the number of treatment beds from 27 to 45, and provides separate treatment areas where the most appropriate care can be given to seniors, families and behavioral patients. Gary Horan, president and CEO of the Elizabeth-based healthcare institution, states, “The overall aim of this project is to not only make the delivery of emergency care more efficient, but also more personal.”
With separate treatment areas, including an expanded “fast track” area for minor emergencies, patients will experience more personalized care tailored to their needs. That level of care will also be delivered more swiftly, thanks to a number of technological innovations. For example, a 128-slice CT scanner, located within the confines of the ER, can produce diagnostic scans in seconds. Previously, patients were transferred out of the ER to the Radiology Department in order to receive a CT or ultrasound scan. This necessitated a ride on a stretcher down long corridors and on an elevator – things that amounted to delay in treatment.
Three new Intensive Care Unit rooms are also part of the project. “We’re doing everything possible to treat patients as quickly as possible in the ER; we certainly don’t want them to wait for a bed in the hospital to open up if they need to be admitted,” Horan says.
Related Articles: